What Insurance Covers Zepbound? A Guide to Understanding Your Options
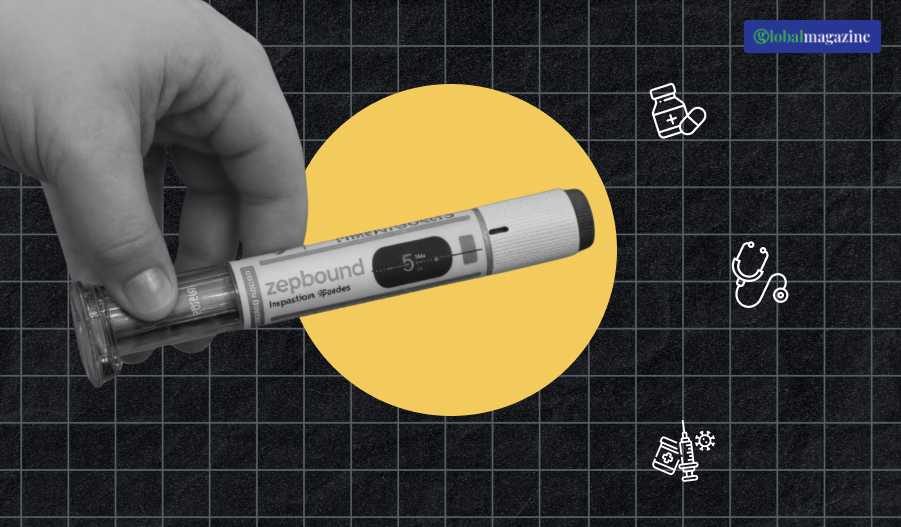
Zepbound is arguably the most widely discuss drug of the day, most particularly about weight control and metabolic illness.
Because there is increasing reliance on drugs to help with chronic conditions such as obesity and diabetes, data regarding the cost and insurance coverage of medications such as Zepbound become increasingly valuable.
As huge as the cost of drugs such as this one is, insurance coverage plays a significant function in determining availability and affordability.
This in-depth review provides comprehensive information on Zepbound insurance coverage. From its mechanisms, to what determines its approval, and how to best maximize your chances of having it covered, this article has you covered.
It even breaks down the cost of Zepbound with insurance and includes actionable advice on navigating the otherwise-sophisticated health insurance process.
What is Zepbound Insurance Coverage?

Zepbound, as with all prescription drug, is eligible under the prescription drug benefit part of health insurance coverage.
Your insurance company will consider a list of criteria when your doctor prescribes Zepbound as to whether it is medically necessary and if it is included in your policy.
Insurers generally take the following into account:
- FDA Approval: Zepbound needs to be FDA-approved for the medical condition for which it is being prescribed, i.e., chronic weight management.
- Indications and Guidelines: The medication should be prescribed for an accepted medical condition and backed by clinical or professional medical association guidelines.
- Formulary Status: Insurers have a formulary containing their tiered list of drugs. Where Zepbound falls on the formulary determines coverage and out-of-pocket costs to a large degree.
- Prior Authorization: Prior authorization with certain insurers, where your physician has to complete forms certifying that the drug is medically indicates, before Zepbound is refilled at the pharmacy.
- Step Therapy: Insurers can adopt step therapy, in which patients must first try more economical drugs. Only if this is not acceptable will the insurer approve Zepbound.
Your coverage can also vary depending on whether you are privately covering, or covering under Medicaid, or under Medicare. Your employer-sponsored coverage can be superior because your employer negotiates.
Why do Some Insurance Plans cover Zepbound?

There are good reasons why some insurance plans do cover Zepbound even though it is relatively new and costly:
1. Medical Necessity
Obesity is increasingly regarded as a chronic state of disease that leads to many secondary diseases, including heart disease, type 2 diabetes, and sleep apnea. Insurers pay more for Zepbound if the patient meets specific clinical criteria (e.g., BMI values or comorbidities).
2. Long-term Cost-Effectiveness
Even though it is expensive to initiate, it has evidence that effective weight-loss drugs would pay a big long-term health cost. As payers avoid expensive hospitalizations, surgeries, and disease management, they also gain an upper hand in leveraging Zepbound as a cost-saver.
3. FDA Approval and Clinical Guidelines
Zepbound is FDA-indication-narrowly approves, and most endocrinologists and obesity doctors think it’s a first-line treatment. More recent clinical guidelines now include it as part of the package, so insurance coverage is likely to follow.
Which Insurance Covers Zepbound?
While plans and states differ, and coverage details differ, the following insurance carriers are most likely to include Zepbound on their drug formularies:
- Blue Cross Blue Shield (all but regional plans)
- UnitedHealthcare
- Aetna
- Cigna
- Humana
- Kaiser Permanente
Private vs. Public Insurance
- Private Insurance: Marketplace and employer-sponsored plans are generally more liberal in freedom, particularly if the plan is premium-tier.
- Medicare and Medicaid: More restrictive in what they cover and may require more documentation in medical necessity evidence. State Medicaid may entirely exclude weight loss medication.
It’s better to read through your insurance policy’s small print or simply talk to an agent to review Zepbound coverage and approval processes.
Determinants of Zepbound Coverage Decisions

Insurers weigh a variety of clinical, fiscal, and policy considerations to determine whether or not to cover Zepbound:
1. Diagnosis and Clinical Reason
- Your physician will need to decide whether Zepbound (e.g., chronic obesity with a BMI of greater than 30 or greater than 27 with comorbidities) is under warranty.
2. Treatment History
- Patients must give a history of past efforts at weight loss on diet and other medications.
3. Medical Necessity Letter
- A physician’s signed letter stating the rationale for prescribing Zepbound will facilitate the approval process.
4. Tier and Formulary Status
- If a higher tier drug is Zepbound, then it can be subjected to greater copays or coinsurance. The lower-tier drugs must try it out first.
5. Type of Plan and Sponsored Employer Benefits
- Private group health plans of private employers (especially large employers) can have more comprehensive coverage or lower prices on newer medicines.
How Much Does Zepbound Cost with and Without Insurance?

1. Zepbound Cost with Insurance
The out-of-pocket price of Zepbound will vary depending on the provisions of your medical insurance:
- Copay Plans: Copays per month can cost between $25 and $75, depending on the formulary tier.
- Coinsurance Plans: You could contribute 10–30% of the medication’s retail price, which would be $100–$300 monthly.
- High-Deductible Plans: You will contribute the entire retail price until you meet your deductible.
2. Zepbound Cost Without Insurance
Without insurance, the cash price for Zepbound is usually $800 to $1,200 monthly, pharmacy, dosage, and state law depending.
3. Cost Saving Tips
- Manufacturer Coupons: Eli Lilly can offer discount cards for eligible patients.
- Pharmacy Discount Programs: Use GoodRx, SingleCare, or other discount programs to lower costs.
- Patient Assistance Programs: The drug manufacturer can offer these for eligible low-income patients.
How to Get Zepbound Covered by Your Insurance
It is challenging to obtain coverage for Zepbound under your medical insurance plan. Follow the below step-by-step actions to enhance your prospects:
- Check Plan Formulary: Verify if Zepbound is included in your plan’s formulary.
- Schedule a Medical Consultation: Your physician must review your medical history and eligibility.
- Obtain Prior Authorization: Assist your physician in acquiring the necessary forms and documents to be submitted to your insurer.
- Add a Letter of Medical Necessity: A doctor letter confirming medical necessity for Zepbound will be useful.
- Track Application Status: Monitor your insurance company and physician to follow up on ongoing paperwork.
- Send Appeal if Rejected: Start a formal appeal and provide documentation on the rejection of coverage.
- Monitor Tier Exception Requests: Requests to the insurance provider to substitute a high-tier drug with a lower-tier drug.
- Use Pharmacy Coupons or Help Programs: Minimize out-of-pocket cost pending approval.
Alternative Options If Zepbound Is Not Covered
If your insurance is not covering Zepbound or is not financially feasible, try the following:
1. Alternative Prescription Drugs
- Wegovy (semaglutide)
- Ozempic (semaglutide)
- Mounjaro (tirzepatide)
- Saxenda (liraglutide)
The substitutes could have different levels of insurance coverage and the same measurements.
2. Generic or Lower-Priced Brands
Look for generic, older weight loss medications that your plan covers.
3. Retail Pharmacy Savings Programs
Walmart and Costco, the large box stores, may have lower prices or in-store sale price discounts.
4. Clinical Trials
Discover Zepbound clinical trials where you may receive the medication for free.
5. Lifestyle Modification Programs
Covered supervised weight loss programs can be supplemented with counseling, nutrition counseling, and exercise training.
Ruminations regarding Zepbound Coverage

As more people develop diseases such as obesity, insurers started to rethink insuring medication. Zepbound, being efficacious, is a drug that patients and physicians would prefer to utilize. But cutting through the insurance barriers isn’t always simple.
Medical coverage varies significantly in terms of what and how much patients pay, and patients need to be proactive, assertive, and persistent.
Prior authorization, appeals, and manufacturer discounts can be beneficial in increasing the likelihood of obtaining Zepbound at a reasonable cost.
Looking Ahead to Insurance Coverage!
The drug’s coverage landscape continues to evolve. Additional clinical data, changing guidelines, and favorable pricing can persuade additional payers to add Zepbound to their formularies. Patients must keep track of their insurance plans during yearly open enrollment to determine if they can make improvements.
Ultimate Tip: Organize by photocopying all relevant forms, including the physician’s note, prior authorization form, denial letter, and appeal request, to streamline the process and increase your chances of approval.
Disclaimer: The article is provided for informational use only and shall not be utilized as insurance or medical guidance. Always consult your healthcare physician and insurance administrator for the most accurate and up-to-date information.

























